“Blood Pressure Spike: Can Fasting Raise It?”
In the ongoing conversation about the benefits and drawbacks of fasting, the spotlight has often landed on its impact on cardiovascular health, and more specifically, on blood pressure. While proponents hail fasting as a panacea for well-being, researchers are now probing deeper into the nuances, questioning if this practice can unexpectedly cause blood pressure to rise. This article intends to sift through the latest findings to unravel the connection between temporary abstinence from food and the acute fluctuations in blood pressure readings. With heart health at the core of the discussion, we investigate whether fasting is a friend or foe to our circulatory systems, and what individuals considering fasting should know about the potential risks and rewards. Join us as we explore this complex relationship, tapping into scientific studies, expert opinions, and real-world data that shed light on the question: Can fasting raise your blood pressure?
Table of Contents
- Understanding Blood Pressure: The Basics Before Fasting
- The Impact of Fasting on Cardiovascular Health
- Investigating the Link Between Fasting and Blood Pressure Fluctuations
- Mechanisms Behind Blood Pressure Increases During a Fast
- Assessing the Risks: Who Should Be Cautious About Fasting
- Dietary Recommendations to Manage Blood Pressure While Fasting
- Navigating the Research: What Studies Say About Fasting and Hypertension
- Expert Insights on Preventing Blood Pressure Spikes During Fasting
- Lifestyle Modifications to Support Healthy Blood Pressure Levels
- Practical Tips for a Safe Fasting Experience for Hypertensive Individuals
- Q&A
- In Summary
Understanding Blood Pressure: The Basics Before Fasting

When we talk about blood pressure, we’re referring to the force exerted by our blood against the walls of our arteries as it circulates throughout our body. It’s a vital health indicator often summarized by two numbers: the systolic pressure, the higher number indicating the pressure during heartbeats; and diastolic pressure, the lower number representing the pressure when the heart rests between beats.
Normal blood pressure levels typically read at or below 120 mmHg systolic and 80 mmHg diastolic. Prehypertension and hypertension stages increase progressively from these numbers. Understanding these ranges is crucial before considering any dietary changes, such as fasting, which might impact these levels.
Fasting, particularly when done for extended periods, can trigger various physiological responses. It often leads to a decrease in the body’s insulin levels and a corresponding rise in the release of stress hormones such as adrenaline and noradrenaline. These hormones are known to constrict blood vessels, leading to a temporary increase in blood pressure. Here’s a simple breakdown of the process:
- Insulin levels drop
- Stress hormones increase
- Blood vessels constrict
- Blood pressure potentially rises
Although the relationship between fasting and blood pressure is complex, research suggests that intermittent fasting may have a long-term lowering effect on blood pressure. However, initially, individuals might experience spikes in blood pressure due to hormone fluctuations. It’s imperative to consult with a healthcare provider who can monitor these changes, especially for those already managing high blood pressure.
| Category | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|---|---|
| Normal | ≤ 120 | ≤ 80 |
| Elevated | 120-129 | ≤ 80 |
| Hypertension Stage 1 | 130-139 | 81-89 |
| Hypertension Stage 2 | ≥ 140 | ≥ 90 |
| Hypertensive Crisis | ≥ 180 | ≥ 120 |
The Impact of Fasting on Cardiovascular Health
When we think about dietary interventions to improve heart health, fasting often enters the conversation. Intermittent fasting, in particular, has gained traction as a means to not only shed pounds but also to potentially provide cardiovascular benefits. It’s posited that fasting can improve blood pressure, a critical marker for cardiovascular well-being. However, it’s not a one-size-fits-all result, and the body’s initial response to fasting could be multifaceted.
Physical Adaptation to Fasting
- Short-term Effects: Initially, the body may experience a sympathetic nervous system response, sometimes leading to a temporary elevation in heart rate and blood pressure. This reaction is typically part of the ‘fight or flight’ response, as the body mobilizes energy reserves.
- Long-term Adaptation: Over time, fasting may lead to weight loss and improved metabolic profiles, which can contribute to better blood pressure regulation and a decrease in overall cardiovascular strain.
Deeper insights into fasting’s effects on heart health stem from both clinical observations and research studies. Evidence suggests that fasting can lead to a reduction in ‘bad’ LDL cholesterol and triglycerides, which may help in the prevention of plaque buildup in the arteries. Furthermore, improvements in the elasticity of blood vessels have been recorded, which can aid in maintaining a healthy blood pressure level during periods of both rest and physical stress.
| Parameter | Before Fasting | After Fasting |
|---|---|---|
| LDL Cholesterol | High | Lowered |
| Triglycerides | High | Reduced |
| Blood Pressure | Variable | Generally Improved |
Despite the promising indicators, it’s important to consider individual health conditions and to consult with a healthcare provider before embarking on a fasting regimen, especially for those with existing heart issues. The nuances of how fasting impacts blood pressure can depend on numerous factors, including the duration and type of fasting protocol, baseline health status, and concurrent medical treatments. Therefore, while fasting might offer cardiovascular benefits for some, it could pose risks for others.
Investigating the Link Between Fasting and Blood Pressure Fluctuations
In our quest to unravel the effects of fasting on our cardiovascular system, recent studies have painted a fascinating picture. While fasting has been hailed for its benefits ranging from weight loss to improved metabolic health, its impact on blood pressure has become a hot topic of research. It’s important to understand how the abstention from eating for extended periods might influence blood pressure levels.
Fasting introduces our bodies to a unique metabolic state. During this period, after the initial adjustment, our insulin levels decrease, and fat cells release their stored sugar to be used as energy. This is believed to contribute to weight reduction and lipid profile improvements, which are associated with better blood pressure control. However, the first few days of fasting could potentially cause stress on the body, which may temporarily raise blood pressure.
- Decrease in insulin levels leading to fat breakdown
- Release of adiponectin, which may support vascular health
- Increase in sympathetic nervous system activity in the initial days
When it comes to blood pressure, there are two key numbers to consider: Systolic and diastolic pressure. Fasting has been shown to affect these differently. For instance, some individuals experience a moderate decrease in systolic blood pressure after several days of fasting, while the diastolic pressure may remain the same or slightly decrease. Body composition, levels of physical activity, and baseline metabolic health all play significant roles in these outcomes.
| Timeframe | Systolic Pressure Change | Diastolic Pressure Change |
|---|---|---|
| First 24 hours | Possible temporary increase | Minimal change |
| 2-7 days | Decrease in many individuals | Stays the same or slight decrease |
| Extended fasting | Variable, dependent on individual health | Variable, dependent on individual health |
Nevertheless, the relationship between fasting and blood pressure is complex and individual responses can vary. Factors such as overall diet quality, stress levels, and sleep patterns can also influence how blood pressure responds to fasting. It’s therefore essential for anyone considering fasting as a health strategy to consult with healthcare professionals, especially when dealing with hypertension or any cardiovascular concerns.
Mechanisms Behind Blood Pressure Increases During a Fast
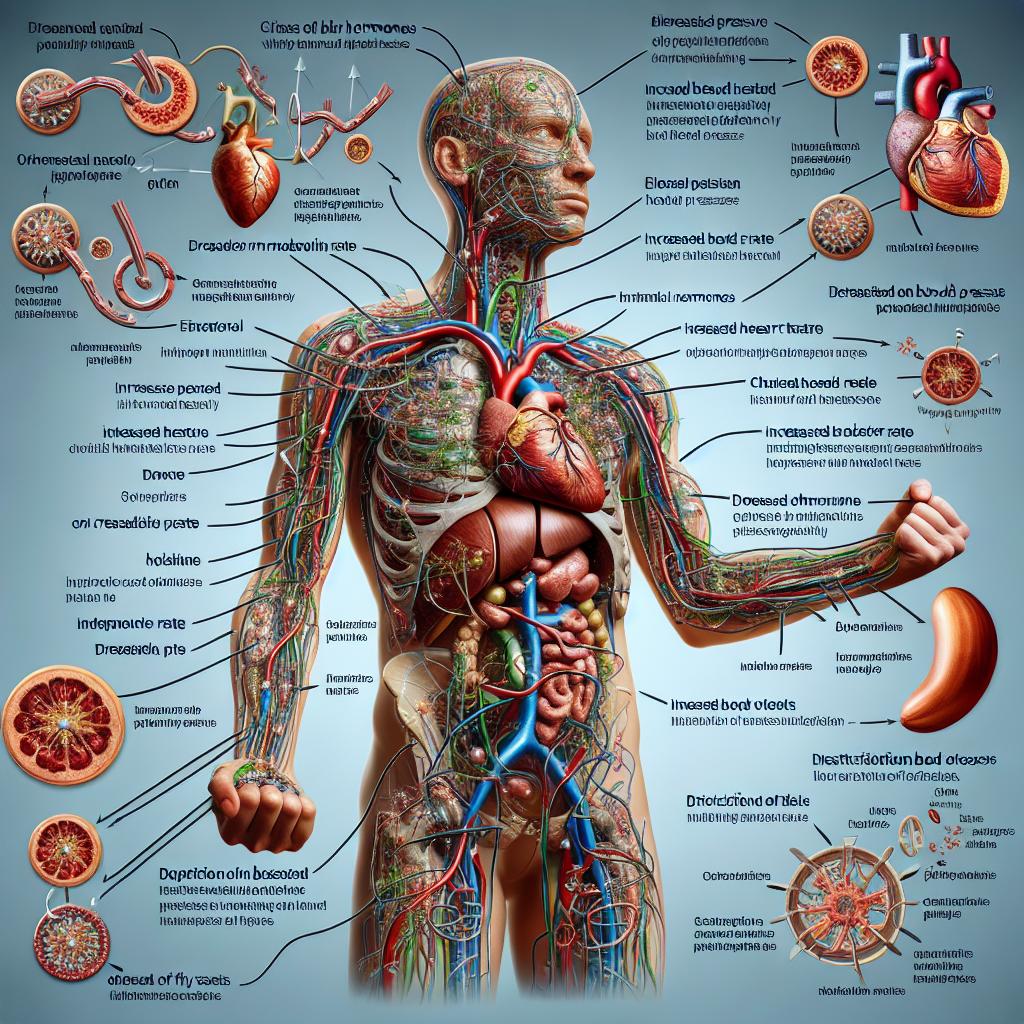
When you embark on a fasting journey, your body goes through various changes, affecting many physiological systems. One such system is our cardiovascular function, where alterations in blood pressure can be observed. Interestingly, despite fasting being touted for its blood-pressure-lowering effects for many, some individuals might experience the opposite. Let’s into the reasons behind these surprising surges in blood pressure during a fast.
The first factor to consider is the fluid balance. Fasting, particularly when it does not include consuming adequate fluids, can lead to dehydration. In response, the body releases stress hormones, such as cortisol and adrenaline, which cause the blood vessels to constrict and, in turn, hike up the blood pressure.
- Fluid Retention: The body might hold on to sodium to compensate for the lack of food intake, leading to fluid retention and increased blood volume.
- Hormonal Fluctuations: Fasting can trigger the release of hormones that influence vascular resistance and heart rate, both of which affect blood pressure readings.
Another consideration is the balance of electrolytes. Fasting impacts the way the body manages electrolytes like sodium and potassium, which play crucial roles in regulating blood pressure. A shift in their ratios can lead to vascular alterations affecting the pressure at which blood is pumped through the circulatory system.
| Electrolyte Imbalance | Possible Effect on Blood Pressure |
|---|---|
| Reduced Potassium | Can cause the body to hold onto sodium, increasing blood pressure. |
| Increased Sodium | May result in fluid retention, adding pressure to blood vessels. |
Fasting can also lead to a temporary increase in fat metabolites in the bloodstream. As the body switches to burning fat for energy due to the absence of food, substances known as ketones can accumulate. Ketones, while an efficient energy source, can also influence blood pressure levels. Additionally, the process of breaking down fat for fuel might lead to an increase in free fatty acids in the blood, which has been linked with stiffening of the arteries and higher blood pressure.
- Ketosis: Fasting-induced ketosis can potentially raise blood pressure by altering blood vessel function and fluid balance.
- Free Fatty Acids: The presence of these acids can reduce the availability of nitric oxide, a molecule essential for regulating vasodilation and blood pressure.
In summary, while fasting can usher in a myriad of health benefits, it’s crucial to recognize that it can also prompt a rise in blood pressure for some. Thorough understanding and monitoring of one’s health, along with professional guidance, can help mitigate these risks and maximize fasting’s positive effects.
Assessing the Risks: Who Should Be Cautious About Fasting
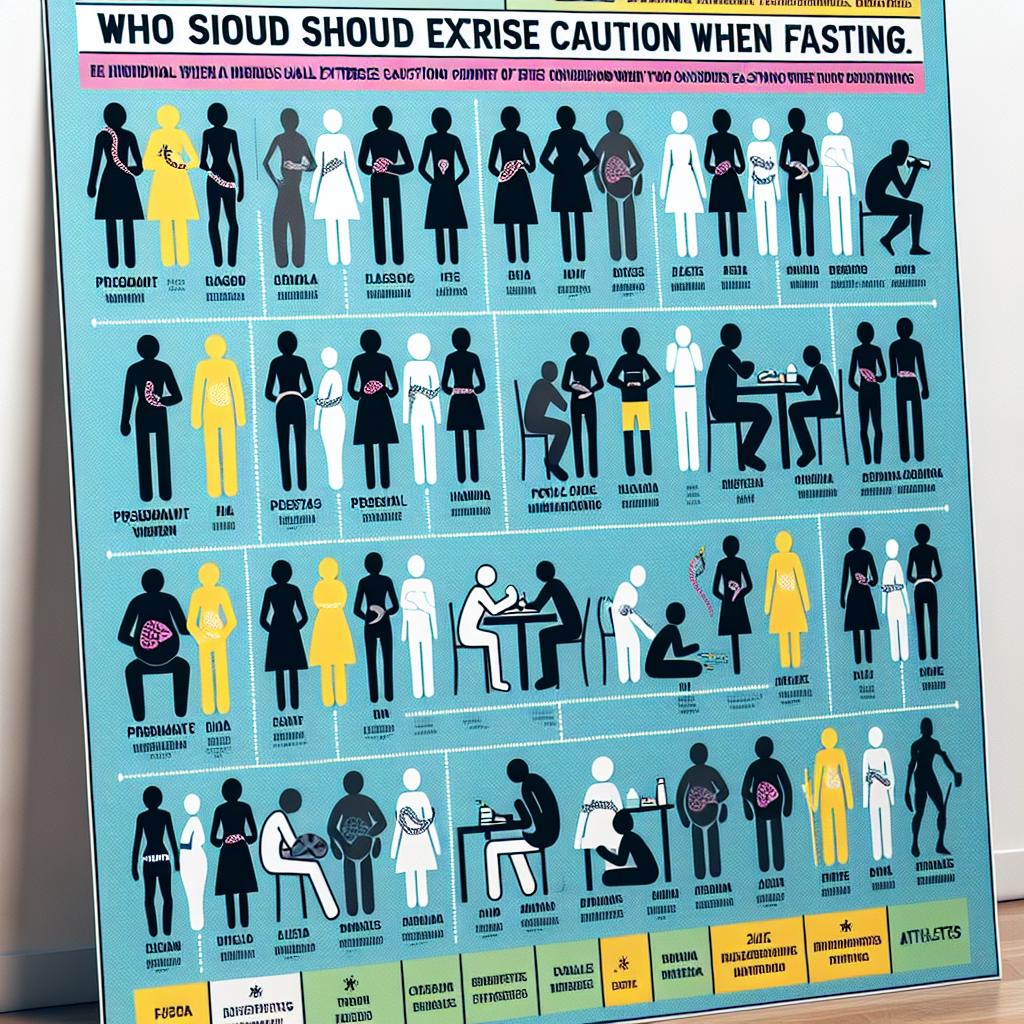
Certainly, fasting has gained recognition for its potential health benefits, but it is important to recognize that it’s not a one-size-fits-all solution. Certain individuals should proceed with caution before adopting any fasting regimen. Focusing on the possible risks, particularly regarding blood pressure, can help guide who might need to be more mindful or avoid fasting altogether.
Individuals with Hypertension or Heart Conditions:
Those with existing high blood pressure or diagnosed heart conditions should approach fasting with considerable caution. The shifts in electrolytes that can occur during fasting might lead to unstable blood pressure levels. It is crucial for these individuals to consult with their healthcare provider before beginning a fasting routine. Monitoring by a medical professional is essential to avoid any exacerbating cardiovascular risks.
People Taking Medication:
Many medications require food intake to ensure proper absorption or to reduce the risk of gastrointestinal irritation. Diuretics or blood pressure medications, in particular, can interact with a fasting state to potentially cause a spike in blood pressure due to changes in kidney function and electrolyte balance. Anyone on medication should negotiate fasting periods carefully with their doctor.
Pregnant or Breastfeeding Women:
From a biological standpoint, fasting is typically not recommended for pregnant or breastfeeding women. The nutrient and energy demands during these periods are heightened, not just for the mother’s health, but also for the developing baby or the quality of breast milk. Any form of calorie restriction could inadvertently affect fetal growth or milk production.
For those considering fasting, understanding personal health conditions and unique risks is paramount. Below is a simplified table highlighting who should reconsider fasting or seek medical advice before starting:
| Group | Consultation Needed | Notes |
|---|---|---|
| Patients with cardiovascular disease | Yes | High risk of adverse effects |
| Individuals on medication | Yes | Drug-nutrient interactions possible |
| Pregnant/Breastfeeding women | Yes | Nutrient requirements increased |
| Those with diabetes | Yes | Risk of hypoglycemia or ketoacidosis |
In conclusion, while fasting can be a powerful tool for health optimization in some, it requires thorough assessment and often medical oversight for others. It’s not merely a dieting trend but a significant lifestyle alteration that may yield diverse physiological responses depending on the individual’s health status.
Dietary Recommendations to Manage Blood Pressure While Fasting

Fasting, a practice that dates back centuries, is often adopted for spiritual, health, or dietary reasons. However, those with concerns about blood pressure should approach fasting cautiously. The body reacts to the lack of food intake during fasting periods, which can lead to fluctuations in blood pressure. To manage this, specific dietary considerations should be kept in mind.
Nutritional balance is crucial when breaking a fast. Emphasize foods rich in potassium, such as bananas, oranges, and leafy greens. Potassium helps mitigate the impact of sodium in the body, which can reduce blood pressure levels. Equally important is to ensure adequate magnesium and calcium intake, found in nuts, seeds, and dairy products. These minerals work together to support healthy blood pressure.
- Avoid high-sodium foods that can exacerbate hypertension, aiming instead for whole foods.
- Stay hydrated with water, as well as drinks that can replenish electrolytes without added sugars or artificial ingredients.
- Consume small, balanced meals that include a mix of complex carbohydrates, lean proteins, and healthy fats upon breaking the fast.
Consulting with healthcare providers before undertaking a fasting regimen is essential, especially for individuals with pre-existing health conditions. Creating a personalized plan that includes safe fasting methods and appropriate dietary choices can help in managing blood pressure effectively during such periods.
| Food Category | Options to Include | Options to Avoid |
|---|---|---|
| Fruits and Vegetables | Spinach, Avocado, Sweet Potatoes | Canned vegetables with added salt |
| Proteins | Chicken breast, Lentils, Fish | Processed meats, High-sodium canned beans |
| Dairy | Yogurt, Skim milk, Cottage cheese | Full-fat cheeses, Cream-based products |
Through conscious planning and informed dietary choices, you can maintain and potentially improve your blood pressure during fasting. The key lies in understanding the body’s needs and responding with appropriate nutrition. By following these guidelines, fasting can be a safe practice, contributing to both physical and spiritual well-being.
Navigating the Research: What Studies Say About Fasting and Hypertension

When exploring the intricate relationship between fasting and blood pressure, there’s a wealth of research that s into the physiological reactions and long-term impacts of this practice. The effects of fasting are nuanced and often depend on how it’s incorporated into one’s lifestyle. For instance, some intermittent fasting studies suggest potential benefits for hypertension, proposing that regular periods without food intake could aid in regulating blood pressure.
These findings align with research that indicates a possible reduction in systolic and diastolic blood pressure among those who engage in short-term fasting. However, it’s essential to note that the benefits may not be universal, with outcomes varying based on individual health profiles and the specifics of their fasting routine. The underlying mechanisms are believed to involve improvements in body weight, insulin sensitivity, and lipid profiles, ultimately influencing blood pressure levels.
- Weight loss associated with controlled fasting periods
- Improved insulin sensitivity potentially reducing hypertension risks
- Alterations in lipid profiles that favor cardiovascular health
Conversely, some studies caution that fasting, particularly when extended or not carefully monitored, can temporarily elevate blood pressure. This phenomenon may possibly be attributed to stress responses elicited by sudden changes in diet. Heightened levels of stress hormones like cortisol have been implicated in short-term increases in blood pressure during fasting periods. It’s crucial, therefore, for individuals with hypertension or those at risk to consult healthcare professionals before embarking on a fasting regimen.
| Type of Fasting | Effect on Systolic BP | Effect on Diastolic BP |
|---|---|---|
| Intermittent | May decrease | May decrease |
| Short-term | Varies | Varies |
| Extended | May increase temporarily | May increase temporarily |
It is clear that while fasting may offer some advantages for those dealing with high blood pressure, the research encourages a personalized approach. The decisive factors often rest in the duration and frequency of fasting, as well as the individual’s overall health condition. Attention to bodily responses and professional guidance can help navigate the mixed research findings, ensuring that fasting is integrated in a way that is safe and potentially beneficial for managing hypertension.
Expert Insights on Preventing Blood Pressure Spikes During Fasting

Embarking on a fasting journey can have considerable health benefits, but it’s crucial to monitor how it may influence your blood pressure. Health experts suggest that significant changes in eating patterns, such as those experienced during intermittent fasting, may lead to unexpected variations in blood pressure. These effects stem from complex interactions between fasting-induced hormonal changes, fluid and electrolyte balance, and individual cardiovascular responses.
Recognizing the Signs of Hypertension is fundamental during fasting. Common signs, albeit sometimes subtle, include headaches, shortness of breath, and nosebleeds. However, many individuals with high blood pressure experience no symptoms at all, making regular monitoring essential. Fasting may mask the typical cues that the body gives when blood pressure is elevated, so keeping a close eye through regular checks is advised.
- Stay Hydrated: Dehydration can occur during fasting, potentially leading to increased blood pressure.
- Mind Your Minerals: Maintaining a balance of essential minerals like potassium and magnesium, which may be depleted during fasting, is crucial.
- Break Your Fast Gently: Choose foods that are easy on the cardiovascular system, avoiding large meals that can cause a significant blood pressure surge.
Strategic Nutritional Considerations should be made to prevent spikes in blood pressure. Nutritional experts recommend the inclusion of certain foods during non-fasting periods to maintain optimal blood pressure levels. Foods rich in potassium, such as bananas and sweet potatoes, help regulate blood pressure. Omega-3 fatty acids found in fish like salmon can also provide cardiovascular benefits.
| Food Group | Examples | Benefits |
|---|---|---|
| Fruits | Bananas, Avocados | Rich in Potassium |
| Leafy Greens | Spinach, Kale | High in Magnesium |
| Proteins | Salmon, Walnuts | Contains Omega-3 Fatty Acids |
In summary, while fasting has its benefits, it is important to approach it with a strategic plan for managing blood pressure. Consulting healthcare professionals before beginning a fast, regular monitoring, and making informed dietary choices can greatly influence the experience, turning it into a healthy, fulfilling journey rather than a health risk.
Lifestyle Modifications to Support Healthy Blood Pressure Levels

Embarking on a journey to manage blood pressure is not solely about medication; it often involves holistic lifestyle changes that can have a significant impact on cardiovascular health. Chief among these changes is dietary adjustment. Embracing a diet rich in fruits, vegetables, whole grains, and lean proteins while cutting back on sodium, processed foods, and excessive fats can be pivotal in lowering and maintaining optimal blood pressure figures.
Physical activity, another cornerstone of heart health, deserves careful attention. Regular exercise, such as brisk walking, cycling, or swimming, can strengthen the heart and improve its efficiency at pumping blood. This physical endeavor works wonders, often leading to a natural reduction in blood pressure levels. Aligning with healthcare providers on a suitable exercise regimen ensures that activities complement individual health statuses and abilities.
- Adequate Sleep: The power of a good night’s sleep on blood pressure cannot be overstated. Aim for 7-9 hours per night to allow the body to regulate stress hormones and maintain a calm and rested state.
- Stress Management: Incorporating mindfulness, yoga, or even simple breathing exercises into daily routines helps mitigate stress, a known contributor to hypertension.
- Moderation in Alcohol: Limit alcohol intake to moderate levels as excessive consumption can elevate blood pressure.
| Activity | Frequency | Benefits for Blood Pressure |
|---|---|---|
| Brisk Walking | 30 min/day, 5 times/week | Improves heart strength and efficiency |
| Yoga | 1 hour/session, 3 times/week | Encourages relaxation and stress relief |
| Strength Training | 20-30 min/session, 2 times/week | Builds muscle, enhances metabolic rate |
Avoiding tobacco and minimizing caffeine intake are additional strategies that render powerful results. Smoking cessation is vital, as nicotine triggers a temporary but dangerous increase in blood pressure, while caffeine can have a more varied effect on individuals. Monitoring these two factors is especially beneficial for those with pre-existing hypertension or those at risk of developing it. The cumulative effect of these proactive choices fosters an environment within the body that favors stable, healthy blood pressure levels.
Practical Tips for a Safe Fasting Experience for Hypertensive Individuals

When considering fasting, especially for those with hypertension, careful planning and consultation with a healthcare provider are crucial. Here are some measures you can take to ensure a safer fasting experience:
- Consult Your Doctor: Before you begin, it’s vital to speak with your physician about your plans to fast. They can provide guidance based on your health, medication, and risk factors, ensuring that your blood pressure remains stable during your fasting period.
- Monitor Your Blood Pressure: Keeping track of your blood pressure levels throughout the fasting period helps detect any significant changes early. Regular monitoring can guide whether you should continue fasting or if adjustments to medication or diet are required.
- Stay Hydrated: Dehydration can lead to a temporary rise in blood pressure. Despite the abstinence from food, ensure you drink sufficient water if your fasting regimen allows it, particularly during non-fasting hours.
- Balanced Meals: During non-fasting periods, focus on heart-healthy foods rich in fruits, vegetables, lean proteins, and whole grains to help maintain normal blood pressure.
Medication timings might need to be adjusted to fit your fasting schedule. This should always be done under the guidance of a healthcare professional. Let’s deeper into the dietary considerations:
| Foods to Include | Foods to Avoid |
|---|---|
| Potassium-rich foods (e.g., bananas, sweet potatoes) | High-sodium foods (e.g., processed meats, canned soups) |
| Omega-3 fatty acids (e.g., salmon, flaxseeds) | High-sugar foods (e.g., pastries, sugary drinks) |
| Calcium-rich foods (e.g., dairy, kale) | Trans fats (e.g., fried foods, certain margarines) |
| Magnesium-rich foods (e.g., spinach, almonds) | Excessive caffeine (can cause blood pressure spikes) |
Physical activity, although beneficial for blood pressure management, should be approached cautiously during fasting. Light to moderate activities such as walking or yoga can help, but always listen to your body and avoid strenuous exercise that can heighten blood pressure or cause dehydration.
Lastly, be mindful of the symptoms indicating that fasting may be negatively impacting your blood pressure, such as dizziness, blurred vision, or palpitations. In the presence of any unusual or concerning symptoms, it’s imperative to cease fasting and seek medical attention immediately. Remember, the primary goal of fasting should be to improve or maintain your health, not to put it at risk.
Q&A
### Q&A: Does Fasting Have an Impact on Blood Pressure?
**Q: What is the connection between fasting and blood pressure?**
A: Fasting, the practice of abstaining from food for a certain period, can have various effects on blood pressure. Some research suggests that fasting may actually lead to a reduction in blood pressure, attributing this to potential weight loss, improved arterial function, and hormonal changes that favor a decrease in blood pressure. Yet, in some cases, particularly during the initial stages of fasting, some individuals might experience a temporary increase in blood pressure due to stress responses and compensatory mechanisms to maintain energy levels.
**Q: Can fasting cause a spike in blood pressure?**
A: While fasting is often associated with health benefits, including potential blood pressure reduction, there can be instances where blood pressure spikes temporarily. This can be due to the body’s initial counter-regulatory hormones response, such as adrenaline, which can raise heart rate and blood pressure to maintain energy levels in the absence of food. However, these effects are generally transient, and blood pressure often normalizes or decreases with continued fasting.
**Q: Are there specific types of fasting that influence blood pressure?**
A: Yes, there are various fasting methods, such as intermittent fasting, alternate-day fasting, and time-restricted feeding, each with different protocols regarding the timing and duration of food intake. The influence on blood pressure may vary with the type of fasting. Intermittent fasting, for instance, has been shown in some studies to be more effective in reducing blood pressure, partly due to better compliance and associated weight loss.
**Q: Who is at risk for a blood pressure increase while fasting?**
A: Individuals with existing health conditions like hypertension, those taking certain medications, and people with electrolyte imbalances might be more prone to experiencing fluctuations in blood pressure during fasting. It is crucial for anyone with a pre-existing condition to consult with a healthcare provider before starting any fasting regimen.
**Q: How can one minimize the risk of a blood pressure spike when fasting?**
A: To minimize the risk of a blood pressure spike during fasting, it is important to ease into the fasting practice gradually, stay hydrated, and ensure that the diet before and after the fast includes balanced, nutritious meals. Monitoring blood pressure, being mindful of how your body is responding, and seeking professional guidance for personalized fasting protocols can also help manage risks.
**Q: Does breaking a fast impact blood pressure?**
A: Yes, the manner in which a fast is broken can impact blood pressure. Consuming a large, high-sodium meal after fasting can cause a sudden increase in blood pressure. To avoid this, it’s recommended to break a fast with a light, low-sodium meal and to gradually reintroduce larger meals to allow the body to adjust.
**Q: Is it safe for people with hypertension to fast?**
A: People with hypertension should approach fasting with caution and under medical supervision. While some individuals with hypertension may experience benefits, such as weight loss and improved blood pressure control, others might not respond as well. Healthcare providers can offer guidance based on individual health profiles, as well as monitoring and adjusting medication if necessary during fasting periods.
In Summary
In closing, the relationship between fasting and blood pressure is a tapestry of complex physiological responses, one that research continues to unravel. While some studies suggest that fasting can cause a temporary spike in blood pressure due to stress hormones, others highlight its potential for long-term cardiovascular benefits and improved blood pressure regulation. It is vital for individuals considering fasting, especially those with pre-existing health conditions, to consult with healthcare professionals before embarking on such practices. Understanding one’s body response to fasting, adjusting the approach as needed, and maintaining a balanced diet with regular physical activity remain the cornerstones of managing blood pressure effectively. As the scientific community s deeper, future findings will undoubtedly shed more light on this intricate subject, guiding better health choices for those seeking the health benefits of fasting without compromising their blood pressure stability.