“Hypertension Hope: Will Fasting Lower Blood Pressure?”
In the ongoing quest for managing hypertension, a condition that affects a staggering one in four adults globally, medical researchers and health practitioners are perpetually on the lookout for effective lifestyle interventions. Amidst the myriad of dietary and wellness strategies, fasting has emerged as a potential ally in the battle against high blood pressure. While the health conscious have long espoused the virtues of various fasting regimens for detoxification and weight loss, recent scientific inquiries suggest that these periods of voluntary abstinence from food might have a significant impact on cardiovascular health. This article s into the heart of the matter, exploring the intricate relationship between fasting and blood pressure. With leading experts weighing in, and evidence mounting from the frontiers of medical research, we examine the question at the forefront of many minds: Will fasting lower blood pressure? Join us as we unravel this complex health puzzle, providing insights that could herald a new wave of hope for those grappling with hypertension.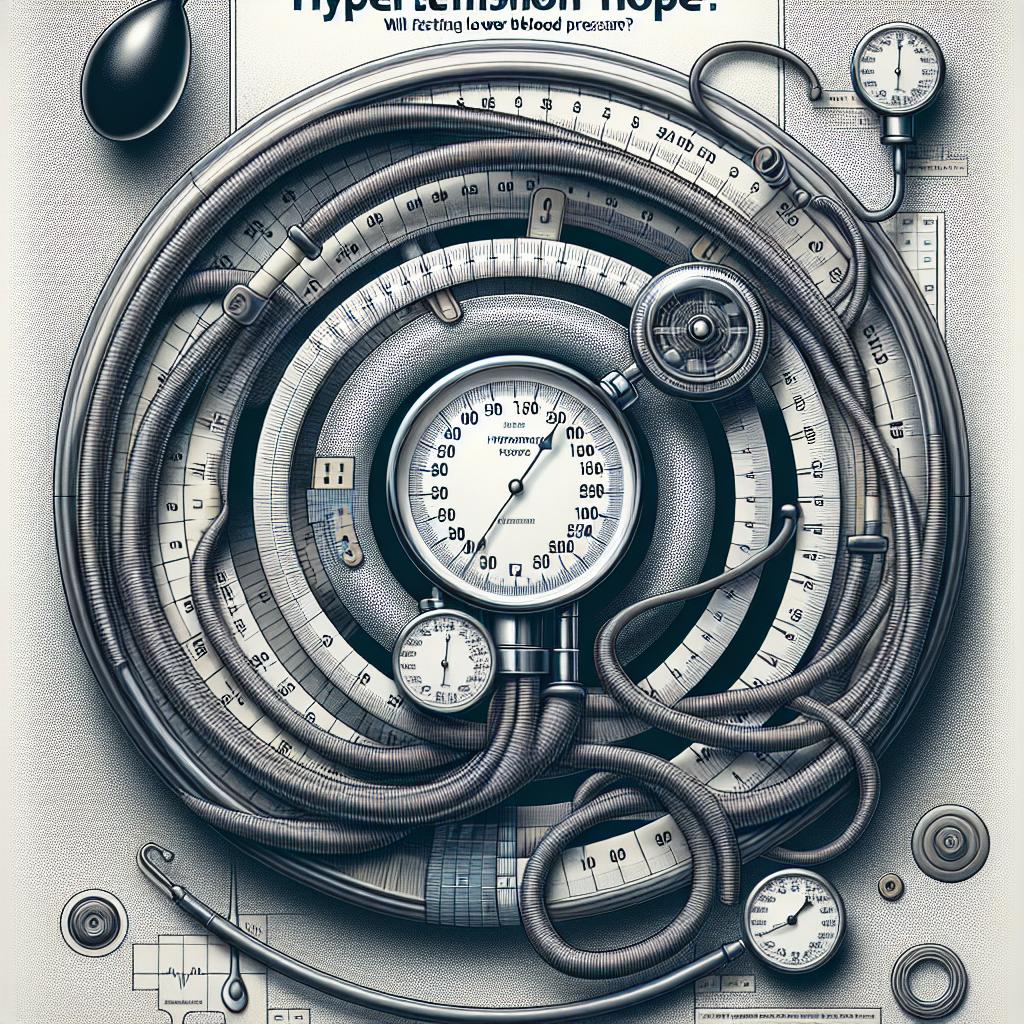
Table of Contents
- Understanding Hypertension: The Silent Killer
- The Fasting Hypothesis: Can Skipping Meals Affect Blood Pressure?
- Exploring the Science: What Research Says About Fasting and Blood Pressure
- The Physiology of Fasting: How the Body Reacts to Short-Term Food Abstinence
- Comparing Fasting Methods: Intermittent Fasting Vs. Prolonged Fasting
- Fasting Safely: Guidelines for Reducing Blood Pressure Without Risk
- Dietary Considerations: What to Eat Before and After Fasts
- Lifestyle and Hypertension: The Role of Exercise and Stress Management
- Personal Stories: Testimonials from Individuals Who Tried Fasting for Blood Pressure Control
- Beyond Fasting: A Comprehensive Approach to Managing Hypertension
- Q&A
- To Conclude
Understanding Hypertension: The Silent Killer

Millions of people worldwide face the challenge of managing high blood pressure, often without any obvious symptoms. This condition can stealthily damage vital organs over time, posing significant health risks if left uncontrolled. With the quest for healthier lifestyles gaining momentum, there is increasing interest in the potential of fasting as a natural intervention to combat this pervasive health issue.
Fasting, the voluntary abstinence from food and drink for a defined period, has long been practiced for spiritual and health reasons. Recent studies have begun to shed light on its physiological benefits, particularly regarding cardiovascular health. For instance, during a fasting state, the body may show improvements in parameters like blood lipid profile, glucose metabolism, and inflammatory markers, which indirectly influence blood pressure levels.
- Reduction in plasma volume
- Decreased sympathetic nervous system activity
- Improved insulin sensitivity
- Weight loss and decrease in adiposity
However, it’s important to acknowledge that the impact of fasting on blood pressure can vary among individuals. The specific type of fasting—be it intermittent, alternate days, or time-restricted eating—can also play a role in how the body responds. To illustrate the varying effects, consider this simple table comparing short-term outcomes for different fasting methods:
| Fasting Method | Average Reduction in Systolic BP (mmHg) | Average Reduction in Diastolic BP (mmHg) |
|---|---|---|
| Intermittent (16/8) | -5 | -3 |
| 24-hour | -10 | -5 |
| Alternate-day | -6 | -4 |
Despite the promise suggested by initial findings, medical experts caution against viewing fasting as a panacea. The practice should not replace proven treatments such as medication and lifestyle changes like regular exercise and dietary adjustments. Moreover, it’s crucial for anyone considering fasting, especially those with pre-existing conditions such as hypertension, to consult with healthcare professionals. Personalized medical advice ensures the safe integration of fasting into one’s overall health strategy.
The Fasting Hypothesis: Can Skipping Meals Affect Blood Pressure?

Exploring the link between fasting and blood pressure is like peering into a complex biological mosaic. The premise is tempting: by restructuring our eating patterns, we might unearth a natural remedy to combat hypertension. But the body’s response to fasting is multifaceted, influencing a cascade of hormonal and physiological changes. One area of interest focuses on insulin sensitivity. Periods of fasting may improve insulin sensitivity, and as a result, can potentially reduce blood pressure, as high insulin levels are linked to hypertension.
Intermittent fasting, which typically involves a cycle of eating and fasting periods over a set schedule, has gained popularity as a potential lifestyle shift to support cardiovascular health. For example, the 16/8 method, where one fasts for 16 hours and eats during an 8-hour window, is often studied. Proponents argue that such a pattern can trigger a process known as autophagy, a cellular “cleanup” that could reduce oxidative stress and inflammation, factors known to influence blood pressure.
- Improves insulin sensitivity and reduces insulin resistance.
- Increases levels of norepinephrine, which can aid in weight loss.
- Initiates autophagy, a cellular repair process.
- May modify the balance of critical electrolytes involved in blood pressure regulation.
Delving into the actual impacts, however, requires skimming through scientific literature for evidence. Initial studies have offered mixed results, making it clear that the answer isn’t as straightforward as we might hope. There are indications that short-term fasting could lead to a temporary reduction in blood pressure, attributed to lower salt intake and alterations in nervous system activity. Yet, it’s critical to differentiate between short-term effects and long-term health outcomes.
| Study | Duration | BP Reduction | Comments |
|---|---|---|---|
| Study A | 8 Weeks | 5 mmHg* | Mild decrease, subjects with mild hypertension |
| Study B | 6 Months | 10 mmHg* | Significant decrease, included diet and exercise |
| Study C | 3 Days | Variable | Short-term fast, mostly water loss |
*systolic BP reduction
To navigate the fasting landscape with confidence, individuals should consider their unique health scenarios and consult with healthcare professionals. While the fasting hypothesis stirs intrigue, it’s not a universal solution and certainly not without its risks. For those with established hypertension, care must be taken to avoid any adverse effects that could arise from dramatic dietary changes. Thus, while we continue to untangle the web of hypotheses and research, a personalized approach remains paramount.
Exploring the Science: What Research Says About Fasting and Blood Pressure

The age-old practice of fasting is being rediscovered through the lens of modern science, particularly concerning its potential health benefits on hypertension. Various research studies have d into how abstaining from food for certain periods might influence blood pressure levels.
One noteworthy study, published in the Journal of Hypertension, examined the relationship between intermittent fasting and its effects on blood pressure. Participants who engaged in periodic fasting showed a reduction in systolic blood pressure. This suggests that fasting could trigger physiological processes that help dilate blood vessels, subsequently lowering the pressure of blood against artery walls.
Moreover, another dimension of research has centered on the impact of fasting on stress hormones like cortisol and adrenaline, which are known to affect blood pressure. The data indicates that fasting may lead to a decrease in stress hormone levels, promoting a more balanced cardiovascular state. This is particularly intriguing, as it opens up possibilities for non-pharmacological interventions in managing hypertension.
- Reduction in oxidative stress
- Improvement in lipid profile
- Modification of circadian rhythms
- Enhanced autophagy and cellular repair processes
Still, it’s essential to approach fasting with caution, as individual responses can vary. Here’s a simplified table summarizing the findings of recent fasting studies:
| Study Focus | Outcome | Participant Profile |
|---|---|---|
| Intermittent Fasting | Lower Systolic BP | Adults with hypertension |
| Stress Hormone Levels | Reduction in Cortisol | Adults at risk for CVD |
| Oxidative Stress Marker | Decreased Levels | Elderly participants |
Conclusively, while research is promising, it is not a one-size-fits-all solution. Healthcare professionals should be consulted before fasting is used as a strategy to combat high blood pressure.
The Physiology of Fasting: How the Body Reacts to Short-Term Food Abstinence

Embarking on a journey of short-term food abstinence, or fasting, takes the body through a fascinating transformation. This process starts with the depletion of glucose stores, primarily found in the liver and muscles. Typically, the body begins to switch energy sources within 8 to 12 hours after the last meal, a metabolic state known as gluconeogenesis. During this phase, the body starts creating glucose using non-carbohydrate sources, such as lactate and amino acids. It’s a clever adaptation that ensures your vital organs get the energy they require in the absence of food.
In the realm of blood pressure management, these adjustments hold potential promise. The body’s natural recourse to fasting triggers a cascade of hormonal responses aimed at conserving energy. Key players include norepinephrine and cortisol, hormones that can influence blood pressure. While norepinephrine tends to increase blood pressure by tightening blood vessels, the reduced calorie intake may lead to lower cortisol levels and a subsequent decrease in blood pressure. Moreover, fasting may enhance the body’s sensitivity to insulin, which can also help in regulating blood pressure.
- Initiation of gluconeogenesis
- Hormonal adjustments to conserve energy
- Decreased sympathetic nervous system activity
- Potential decrease in cortisol production
- Improved insulin sensitivity
The body’s next step in the fasting process involves a gradual move toward burning fat for energy—a phase aptly named ketosis. When carbohydrate consumption plummets, the liver begins to convert fat into ketones, a secondary fuel source that can power almost every cell in the body. Not only does this shift to fat-burning mode have implications for weight control and metabolic health, but it also might affect blood pressure. In ketosis, the body’s insulin levels typically lower, which can result in a significant diuresis, or fluid loss, potentially leading to a decrease in blood pressure.
| Metabolic State | Energy Source | Effect on Blood Pressure |
|---|---|---|
| Gluconeogenesis | Non-carbohydrate substrates | Variable |
| Ketosis | Fatty acids and ketones | Potential decrease |
| Post-fast Re-feeding | Glucose (carbohydrates) | Can increase |
Interestingly, the relationship between fasting and blood pressure is nuanced. Besides hormonal and metabolic changes, fasting may influence the autonomic nervous system, reducing the activity of the sympathetic nervous system—the part often associated with the “fight or flight” response, which can increase blood pressure. Research indicates that short-term fasting might lead to a reduction in overall sympathetic activity, thereby promoting a more relaxed state for the cardiovascular system and potentially lowering blood pressure. Exploring the efficacy of fasting as a natural intervention for hypertension is still an evolving science, but the physiological underpinnings suggest a promising correlation worth further investigation.
Comparing Fasting Methods: Intermittent Fasting Vs. Prolonged Fasting

When it comes to harnessing the potential benefits of fasting for blood pressure reduction, both intermittent fasting and prolonged fasting have gained considerable attention. Let’s into what separates and unifies these approaches.
Intermittent fasting (IF) operates on a cyclical schedule, typically segmenting days or weeks into fasting periods interspersed with eating windows. Common IF methods include:
- The 16/8 method: Fasters consume all their daily calories within an 8-hour window and fast for the remaining 16 hours.
- The 5:2 approach: Individuals eat normally for five days a week but restrict calorie intake to 500-600 calories for the other two non-consecutive days.
- Eat-Stop-Eat: This involves a full 24-hour fast once or twice a week.
Studies suggest that IF may help reduce blood pressure by improving body composition, insulin sensitivity, and circulatory health. For instance, a reduction in body fat, often a byproduct of IF, is linked to lower blood pressure levels due to decreased strain on the heart and arteries.
Prolonged fasting (PF), on the other hand, extends the fasting period beyond the typical IF range, usually for 48 hours or more. During this time, the body may enter a state of deeper metabolic changes, such as:
- Enhanced autophagy, the process by which cells clean out any unnecessary or damaged components.
- Improved hormonal balance, including the regulation of hormones like norepinephrine, which can influence blood pressure.
- Reduction in inflammation, often associated with chronic high blood pressure.
While PF can offer profound health shifts, it necessitates medical supervision, especially for individuals with pre-existing conditions like hypertension.
Emerging evidence underscores the importance of individual responsiveness when comparing the effects of IF and PF on blood pressure. Factors such as age, gender, metabolic rate, and lifestyle habits can significantly sway outcomes. In a clinical study, participants practicing IF demonstrated a modest decline in systolic blood pressure compared to those who did not fast.
| Fasting Method | Average Systolic BP Change | Average Diastolic BP Change |
|---|---|---|
| Intermittent Fasting | -8mmHg | -6mmHg |
| Prolonged Fasting | -12mmHg | -10mmHg |
Although research is promising, it must be stressed that fasting may not be suitable for everyone and can introduce risks if not carefully managed. Anyone interested in trying fasting as a means to control hypertension should consult with their healthcare provider for personalized advice and to ensure a safe and effective approach.
Fasting Safely: Guidelines for Reducing Blood Pressure Without Risk

If you’re considering incorporating fasting into your strategy to tackle high blood pressure, it’s essential to approach it with mindfulness to safeguard your health. Fasting can induce numerous physiological changes, some of which may positively influence blood pressure levels. However, these benefits do not come without risks, particularly for those who have pre-existing health conditions or take medications. Below are key guidelines to help you undertake fasting in a manner that supports your goals while minimizing potential dangers.
- Start with Medical Consultation: Before embarking on any fasting regimen, consult with a healthcare provider, especially if you have hypertension or other medical conditions. Your doctor can help tailor a fasting plan to your specific health needs, ensuring that your medication and nutritional requirements are considered.
- Choose the Right Type of Fasting: There are various fasting methods, such as intermittent fasting (16/8 or 5:2 methods) and time-restricted feeding. Begin with gentle approaches and short fasting intervals to allow your body to adapt slowly.
- Monitor Your Body’s Response: Pay close attention to how your body reacts. Regularly monitor your blood pressure, and be aware of symptoms such as dizziness, weakness, or confusion, which could indicate adverse effects. Adjust your fasting plan accordingly.
- Stay Hydrated and Mind Your Nutrition: Even when not eating, it’s crucial to stay well-hydrated with water, and when you do eat, focus on nutrient-rich foods that support blood pressure health, such as leafy greens, berries, oats, and fatty fish.
Nutritional Intake and Timing Considerations are elements that cannot be overstated. While fasting, your food intake windows matter immensely. Opt for balanced meals that deliver adequate electrolytes, vitamins, and minerals. Incorporate foods high in potassium and magnesium, which are known to support healthy blood pressure levels, and limit your consumption of sodium-rich products.
| Time Window | Food Suggestions |
|---|---|
| Break-Fast | Whole grains, lean proteins, fresh vegetables |
| Last Meal | Fatty fish, salad with olive oil dressing, fruit |
Remember, the goal of fasting is not only to reduce blood pressure but also to enhance overall well-being. Sustainable lifestyle adjustments that include regular physical activity, adequate sleep, and stress management are vital components that complement the efforts of fasting. Fasting should be a part of a holistic approach to health, rather than a standalone quick fix.
In conclusion, while fasting might be a beacon of hope for many battling hypertension, it must be practiced with caution and care. By adhering to these safety guidelines, fasting can potentially be a powerful ally in your journey toward lower blood pressure and improved health. Keep in mind, not everyone will experience the same results from fasting, so it’s crucial to maintain an open dialogue with your healthcare provider and adjust your plan as needed.
Dietary Considerations: What to Eat Before and After Fasts

Embarking on an intermittent fasting journey for blood pressure management prompts a thoughtful consideration of pre- and post-fasting nutrition. The meals you consume surrounding your fasting windows play a pivotal role in maintaining your energy levels and supporting overall health. Here’s what to keep in mind to nourish your body adequately during those critical eating periods.
Before Fasting: To stave off hunger and sustain energy during your fasting period, focusing on foods rich in fiber, protein, and healthy fats is key. Opt for a balanced meal that includes:
- Complex carbohydrates like quinoa or sweet potatoes for a slow-release of energy.
- Lean protein sources such as chicken breast, tofu, or lentils to help you feel satiated.
- Healthy fats from foods like avocados or almonds to promote fullness and fuel your body.
After Fasting: When breaking a fast, it is essential to reintroduce food gently to your digestive system. Start with:
- A small meal that includes easily digestible foods such as fruits like bananas or a portion of cooked vegetables.
- Gradually include proteins and whole grains in subsequent meals to rebuild and replenish your body’s needs.
- Stay mindful of hydration—consuming water-rich foods such as cucumber or watermelon can help rehydrate and reintroduce nutrients smoothly.
In the context of hypertension, it’s also crucial to limit intake of high-sodium foods which can exacerbate high blood pressure. The following table provides a quick reference for sodium-smart choices in your pre- and post-fasting meals:
| Meal Timing | Food Category | Recommended Options | Foods to Avoid |
|---|---|---|---|
| Pre-Fasting | Carbohydrates | Brown rice, oatmeal | White bread, sugary cereals |
| Proteins | Grilled salmon, chickpeas | Processed meats, high-sodium canned beans | |
| Post-Fasting | Fruits & Vegetables | Steamed broccoli, apples | Pickles, canned veggies with added salt |
| Hydration | Herbal teas, water with lemon | Sweetened beverages, alcohol |
Remember, nurturing your body with the right foods before and after fasting can leverage the potential benefits for hypertension control. Always consult with your healthcare provider before initiating dietary changes, especially if you have any pre-existing health conditions or are on medication for blood pressure management.
Lifestyle and Hypertension: The Role of Exercise and Stress Management

When embarking on a quest to regulate hypertension, adopting a heart-healthy lifestyle is pivotal. Integrating regular physical activity into one’s daily routine stands as a cornerstone of managing high blood pressure. Exercise, especially cardiovascular workouts like brisk walking, cycling, or swimming, can help lower blood pressure by strengthening the heart, enabling it to pump blood with less effort, thus reducing the force on arteries. Moreover, routine exercise can aid in maintaining a healthy weight, another significant factor in controlling blood pressure levels.
But it’s not all about physical activity; stress management also plays a crucial role in blood pressure regulation. Chronic stress is a notorious catalyst for transient spikes in blood pressure. While occasional stress-induced increases in blood pressure are natural, prolonged stress without relief may lead to long-term hypertension. Techniques such as deep breathing, meditation, and yoga can be effective tools for stress reduction. They encourage relaxation by activating the parasympathetic nervous system, which in turn decreases heart rate and dilates blood vessels, ultimately leading to lower blood pressure.
The synergy between exercise and stress management is undeniable. A consistent exercise regimen promotes the release of endorphins, the brain’s natural mood lifters, which can alleviate stress. To illustrate their effectiveness, let’s consider the following table representing a simple weekly exercise plan:
| Day | Activity | Duration (Minutes) |
|---|---|---|
| Monday | Brisk Walk | 30 |
| Wednesday | Cycling | 30 |
| Friday | Swimming | 30 |
| Saturday | Yoga | 45 |
Though exercise and stress management form an impressive tandem, they should be complemented by other lifestyle modifications for optimal impact on blood pressure. Balanced diets, moderation in alcohol consumption, and abstinence from smoking work together with these practices to forge a multi-faceted defense against the perils of hypertension. Remember, these changes may not produce instant results, but consistency is key. Over time, they can make marked improvements in both blood pressure readings and overall well-being.
Personal Stories: Testimonials from Individuals Who Tried Fasting for Blood Pressure Control

The relationship between fasting and blood pressure is one that beckons a blend of scientific curiosity and real-life experiences. Anecdotal evidence sprinkles hope across many discussions concerning non-pharmaceutical interventions in managing hypertension. Gloria M. from Texas shares her journey, revealing that intermittent fasting, when paired with moderate exercise, not only helped shed excess pounds but also resulted in a noticeable reduction in her blood pressure over a few months. “It felt like a two-for-one deal on my health,” she remarks.
Akin to Gloria’s experience, Steven K., a retired school teacher from Ohio, recounts his foray into the 5:2 fasting diet, a regimen where caloric intake is significantly reduced for two non-consecutive days a week. “The ‘fast’ days were tough at first, but soon became a habit,” Steven explains. After six months, his systolic blood pressure had fallen by 12 mmHg. To organize his dietary plan, he created a simple table that tracked his weekly progress:
| Week | Systolic BP | Diastolic BP | Notes |
|---|---|---|---|
| 1 | 150 | 95 | Starting point |
| 12 | 142 | 90 | Noticing positive changes |
| 24 | 138 | 85 | Improved readings |
| 36 | 130 | 82 | Reached target BP |
However, it’s imperative to note that individual results can vary widely. Natalie P., a freelance designer from California, faced quite different results. She admits, “My blood pressure remained high despite religious adherence to a 16:8 fasting schedule.” Her testimony is a candid reminder that fasting may not be the silver bullet for everyone’s hypertension journey. Natalie’s experience underscores the importance of a personalized approach to health and the necessity of consulting healthcare professionals.
In their list of stories, readers might also come across Jacob T., who swears by the power of prolonged fasting. He claims it helped tip the scales on his blood pressure, but he stresses the importance of medical supervision:
- Consult with a doctor before starting a fast
- Monitor blood pressure regularly during the fast
- Break the fast if feeling unwell
Jacob’s discipline under expert guidance was crucial in his successful encounter with fasting as a means to manage his hypertension.
Beyond Fasting: A Comprehensive Approach to Managing Hypertension

When exploring the multifaceted strategies for blood pressure management, integrating lifestyle alterations with dietary modifications proves to be a winning combination. Fasting, while often spotlighted for its potential health benefits, is just one aspect of a viable plan to manage hypertension. Studies suggest that intermittent fasting may have a positive impact on blood pressure, but to achieve lasting results, a broader lifestyle approach is essential.
For those considering the incorporation of fasting into their regimen, it’s imperative to understand the spectrum of interventions:
- Regular Physical Activity: Consistent exercise helps maintain a healthy heart and circulatory system, reducing the strain on your blood vessels.
- Stress Reduction Techniques: Practices like meditation, yoga, or deep-breathing can help to lower blood pressure by reducing the stress response in your body.
- Quitting Smoking: Smoking cessation is critical as it decreases the risk of hypertension and improves overall cardiovascular health.
- Limited Alcohol Consumption: Reducing alcohol intake can have an immediate effect on lowering blood pressure levels.
It’s also important to note the influence of nutrition in hypertension management. A carefully crafted diet, rich in fruits, vegetables, whole grains, and low in sodium and unhealthy fats, is key. The DASH diet (Dietary Approaches to Stop Hypertension) is a prime example of an eating plan specifically designed to combat high blood pressure. Emphasizing foods that are high in calcium, potassium, and magnesium—all minerals that aid in blood pressure regulation—this diet serves as a blueprint for healthy eating.
| Element | Importance | Sources |
|---|---|---|
| Calcium | Helps blood vessels tighten and relax when they need to. | Dairy products, leafy greens, almonds. |
| Potassium | Lessens the effects of sodium and eases tension in blood vessel walls. | Bananas, potatoes, tomatoes. |
| Magnesium | Aids in the proper function of hundreds of enzymes and maintains blood pressure. | Whole grains, legumes, seeds, nuts. |
Taking a comprehensive approach to managing hypertension means considering all facets of health. Fasting may serve as a launching point for some, but without the support of additional lifestyle changes, its effects could be transient. Regular health check-ups, monitoring blood pressure at home, and maintaining open communication with healthcare providers complement the commitment to a healthier lifestyle, offering hope and tangible results in the management of hypertension.
Q&A
### Can Fasting Help Lower Blood Pressure?
**Q: What exactly is hypertension?**
A: Hypertension, also known as high blood pressure, is a condition where the force of blood against your artery walls is consistently too high. Over time, this increased pressure can cause health issues, including heart disease and stroke. It’s often referred to as a ”silent killer” because it doesn’t always exhibit noticeable symptoms.
**Q: How prevalent is hypertension?**
A: Hypertension is a common health concern worldwide. According to the World Health Organization, an estimated 1.13 billion people globally suffer from hypertension, and less than 1 in 5 have it under control. This underscores the imperative for effective management strategies.
**Q: What is the scientific basis for considering fasting as a hypertension intervention?**
A: The potential of fasting to lower blood pressure comes from its ability to improve several physiological markers, like insulin sensitivity and lipid profiles, and to promote weight loss. Past research has indicated that intermittent fasting, in particular, may trigger a reduction in blood pressure by influencing these factors.
**Q: What types of fasting might impact blood pressure?**
A: Intermittent fasting, which includes methods like time-restricted feeding where one eats within a specific time window each day, and periodic fasting, where individuals refrain from or significantly reduce calorie intake for entire days, are both areas of investigation in blood pressure research.
**Q: Are there any studies that demonstrate fasting can reduce blood pressure?**
A: Yes, several studies have reported reductions in both systolic and diastolic blood pressure as a result of intermittent fasting. For instance, a 2020 study in the journal ‘Nutrients’ found that intermittent fasting could lead to modest reductions in blood pressure among adults with metabolic syndrome.
**Q: Is fasting safe for everyone with hypertension?**
A: Fasting is not appropriate for everyone. People with advanced hypertension, those who are pregnant, underweight, or have certain medical conditions, and anyone taking medications that require food intake should consult with a healthcare provider before starting a fasting regimen.
**Q: Can fasting replace hypertension medications?**
A: Fasting should not replace medications prescribed for hypertension without a doctor’s guidance. While it may help manage blood pressure, it is not considered a standalone cure and should be part of a broader lifestyle change that can include diet, exercise, and medication as needed.
**Q: How should one start fasting to lower blood pressure?**
A: Fasting should be undertaken carefully and gradually. It’s advisable to start with shorter fasting periods and to be aware of one’s own body reactions. Working with a healthcare provider, who can provide personalized fasting schedules and monitor your health, is crucial.
**Q: What are some potential risks or side effects associated with fasting?**
A: Potential side effects can include dizziness, headaches, low blood sugar (hypoglycemia), and nutrient deficiencies if practiced for extended periods without proper guidance. Monitoring by a healthcare professional is recommended to mitigate these risks.
**Q: What other lifestyle changes can support the benefits of fasting in reducing blood pressure?**
A: Alongside fasting, adopting a balanced diet rich in fruits, vegetables, whole grains, and limiting sodium intake can enhance blood pressure control. Regular physical activity and maintaining a healthy weight are also key components of effective hypertension management.
It’s important to note that while emerging research is promising, fasting as a method to lower blood pressure requires careful consideration and should be managed by healthcare professionals to ensure patient safety and effectiveness.
To Conclude
In conclusion, the potential of fasting as a means to lower blood pressure opens a new chapter in the chronicle of hypertension management. While research suggests there may be a connection between reduced caloric intake and improved cardiovascular health, the dialogue between fasting enthusiasts and medical professionals continues. It is critical for individuals considering this path to consult with their healthcare providers to tailor a plan that considers existing health conditions and lifestyle factors. The promise of fasting must balance optimism with caution—science tells us the solution to hypertension will not be found in quick fixes, but rather in well-informed, clinically supported strategies that prioritize long-term wellbeing. As we turn the page on traditional hypertension therapies, we await further investigations with bated breath. Will fasting lower blood pressure substantially? Only time and rigorous scientific inquiries will tell. But for now, hope is on the horizon for those seeking alternative methods to combat the silent killer known as hypertension.