“Diabetes Detection: What Fasting Blood Sugar Reveals”
Diabetes, a pervasive chronic condition, afflicts millions globally, silently escalating into a formidable public health concern. At the heart of its timely detection lies the fasting blood glucose test—a key metric for assessing the risk and presence of this disease. As we navigate through the labyrinth of modern medicine’s diagnostic tools, the fasting blood sugar level stands as a crucial indicator, offering a window into the body’s intricate balance of insulin and glucose. This article endeavors to unravel the importance of fasting blood sugar in the early detection of diabetes, scrutinizing how this simple yet vital test can illuminate the path to early intervention and management. With a spotlight on the latest research and expert insights, we unfold the narrative of how a fasting blood sugar test not only offers a snapshot of your current health status but also how it can potentially forecast the future of one’s wellbeing.
Table of Contents
- Understanding Fasting Blood Sugar and Its Role in Diabetes Detection
- The Science Behind Fasting Blood Sugar Levels and Glycemic Control
- Normal vs. Elevated Fasting Blood Sugar: Interpreting Your Numbers
- Risk Factors for Abnormal Fasting Blood Sugar and Potential Diabetes
- Pre-Diabetes and Diabetes Thresholds: When to Be Concerned
- The Importance of Consistent Monitoring of Fasting Blood Sugar
- Lifestyle Interventions to Manage Fasting Blood Sugar Levels
- Medical Recommendations for Individuals with High Fasting Blood Glucose
- Advancements in Blood Sugar Testing: Beyond the Traditional Fasting Method
- Taking Action: Steps to Take if Your Fasting Blood Sugar Is High
- Q&A
- The Conclusion
Understanding Fasting Blood Sugar and Its Role in Diabetes Detection

Stepping into the world of glucose monitoring is akin to unlocking the secrets of your body’s energy management system. When we consume food, particularly carbohydrates, our body converts it into glucose, becoming the fuel that powers our day. However, when our internal systems face glitches—like in diabetes—this process is disrupted. Blood sugar tests, particularly the fasting blood sugar (FBS) test, serve as the litmus test for understanding how well this energy conversion and absorption process is doing.
Fasting blood sugar levels are indicative benchmarks used by healthcare professionals to assess glucose handling in our bodies after a period of not eating. It’s a window into how well the pancreas is managing its insulin production and secretion duties. In essence, higher levels of fasting blood sugar suggest that the body is struggling with insulin efficiency, pointing toward diabetes or pre-diabetes. The FBS test is done after an overnight fast, typically requiring the patient to abstain from eating or drinking anything except water for at least 8 hours before the test.
Doctors look for specific ranges when evaluating fasting blood sugar results:
- Normal: 70-99 mg/dL
- Pre-diabetes (impaired fasting glucose): 100-125 mg/dL
- Diabetes: 126 mg/dL or higher on two separate tests
These numbers are not just digits but are crucial for categorizing an individual’s glucose control status and for crafting a potential management or intervention plan.
| Fasting Blood Sugar Levels (mg/dL) | Condition |
|---|---|
| Less than 70 | Potentially Hypoglycemic |
| 70-99 | Normal |
| 100-125 | Pre-diabetes |
| 126 and above | Diabetic Range |
Being well-informed about fasting blood sugar levels is empowering, allowing individuals to make proactive health choices. The outcomes of the FBS test can be a catalyst for lifestyle modifications and medical interventions to restore balance in blood sugar levels. As diabetes is often a silent stalker, regular monitoring of fasting glucose can give timely insights, which is essential in managing or even deterring the progression of diabetes.
The Science Behind Fasting Blood Sugar Levels and Glycemic Control
Understanding the mechanisms of fasting blood sugar is pivotal in comprehending overall glycemic management—a crucial aspect for those monitoring diabetes risk and management. When we fast, typically overnight, our body still requires energy. The liver helpfully releases stored glucose into the bloodstream to provide this energy. Measuring blood sugar after a period of fasting gives us a baseline that indicates how well the body is managing this glucose release without the influence of recent meals.
The role of insulin is to help cells absorb glucose and maintain balanced blood sugar levels. However, in individuals with diabetes, this process doesn’t work as it should due to either insulin resistance or insufficient insulin production. Fasting blood sugar tests thus offer a snapshot of metabolic health: healthy levels suggest the body’s insulin response is functioning adequately, while elevated readings may signify a pre-diabetic or diabetic condition.
Glycemic control is a term that encapsulates how well a person’s blood sugar levels are regulated over time. To illustrate, consider the following simple table that categorizes fasting blood sugar levels:
| Condition | Fasting Blood Sugar Level (mg/dL) |
|---|---|
| Normal | < 100 |
| Pre-diabetes | 100-125 |
| Diabetes | ≥ 126 |
Consistently elevated fasting blood sugar levels can lead to a diagnosis of type 2 diabetes. For this reason, in-depth analysis of factors contributing to these levels is essential: diet, physical activity, stress, and genetics all intertwine to craft a complex physiological tapestry. This intricacy necessitates a personalized approach to glycemic control—a lifestyle tailoring that involves monitoring carbohydrate intake, engaging in regular exercise, managing stress effectively, and appropriate medication when necessary, all under expert guidance.
Normal vs. Elevated Fasting Blood Sugar: Interpreting Your Numbers

Understanding your fasting blood sugar levels is crucial in assessing your risk for diabetes or managing the condition if you’ve already been diagnosed. The fasting blood sugar test, taken after an overnight fast, provides a snapshot of your blood glucose levels and can indicate how your body is processing sugar.
Typical Ranges
A normal fasting blood sugar level is typically between 70 and 99 milligrams per deciliter (mg/dL). When your levels fall within this range, it suggests that your body is managing its glucose well. However, if your readings are consistently higher, it may be a sign that your body is struggling to maintain its blood sugar, which can be an early warning signal for pre-diabetes or diabetes.
- Normal: 70-99 mg/dL
- Elevated (Pre-diabetes): 100-125 mg/dL
- Diabetes: ≥126 mg/dL on two separate tests
Elevated Levels and Health Implications
An elevated fasting blood sugar level, one that is between 100 and 125 mg/dL, is often considered pre-diabetes. This is a serious health flag, indicating that without intervention and lifestyle changes, type 2 diabetes could develop. Beyond the risk for diabetes, elevated blood sugar levels may contribute to heart disease, stroke, and kidney damage.
| Condition | Fasting Blood Sugar Levels (mg/dL) |
|---|---|
| Normal | 70-99 |
| Pre-diabetes | 100-125 |
| Diabetes | ≥126 |
Decoding your numbers becomes a roadmap to better health when understood correctly. If your fasting blood sugar is elevated, it’s essential to consult with a healthcare professional to discuss the necessary steps to manage and potentially reverse this condition. Monitoring dietary choices, increasing physical activity, and possibly medication under medical guidance can significantly impact blood sugar levels and overall well-being.
Risk Factors for Abnormal Fasting Blood Sugar and Potential Diabetes

Understanding your fasting blood sugar levels can be your first line of defense in identifying the risk of prediabetes or diabetes. Factors that influence these levels are numerous, ranging from lifestyle choices to genetic predispositions. Lifestyle choices play a pivotal role; a diet high in refined sugars and processed foods, coupled with a sedentary lifestyle, significantly increases the risk. On the flip side, those who integrate balanced diets and regular exercise into their routine generally see more favorable blood sugar readings.
In the intricate web of risk factors, family history is a strong predictor, revealing a hereditary aspect to the condition. If close relatives have diabetes, your own risk for abnormal fasting blood sugar and potential diabetes rises. Moreover, certain ethnic groups – including African American, Hispanic, Native American, and Asian American – have all been identified as having a higher prevalence of diabetes.
Weight is another critical consideration, as obesity is closely linked with the development of type 2 diabetes. Excess fat, particularly around the abdomen, increases insulin resistance. Age is similarly worth noting; individuals over the age of 45 are advised to test regularly for changes in blood sugar levels, as the risk of developing diabetes increases with age. Additionally, conditions such as polycystic ovary syndrome (PCOS) and a history of gestational diabetes can elevate one’s risk profile. The table below summarizes these key risk factors:
| Risk Factor | Details |
|---|---|
| Diet and Exercise | High intake of sugar, low physical activity |
| Family History | Immediate family with diabetes |
| Ethnicity | Higher prevalence in certain ethnic groups |
| Body Weight | Obesity, especially abdominal fat |
| Age | Increased risk for individuals aged 45+ |
| Other Conditions | PCOS, gestational diabetes history |
It’s not all about external factors; internal health issues can also exert influence. For instance, a diagnosis of hypertension or high cholesterol can indicate an elevated risk for diabetes. This underscores the significance of comprehensive health monitoring. Remember, awareness of these risk factors coupled with regular monitoring of fasting blood sugar can lead to early detection and management of diabetes, potentially staving off its myriad complications and maintaining quality of life.
Pre-Diabetes and Diabetes Thresholds: When to Be Concerned
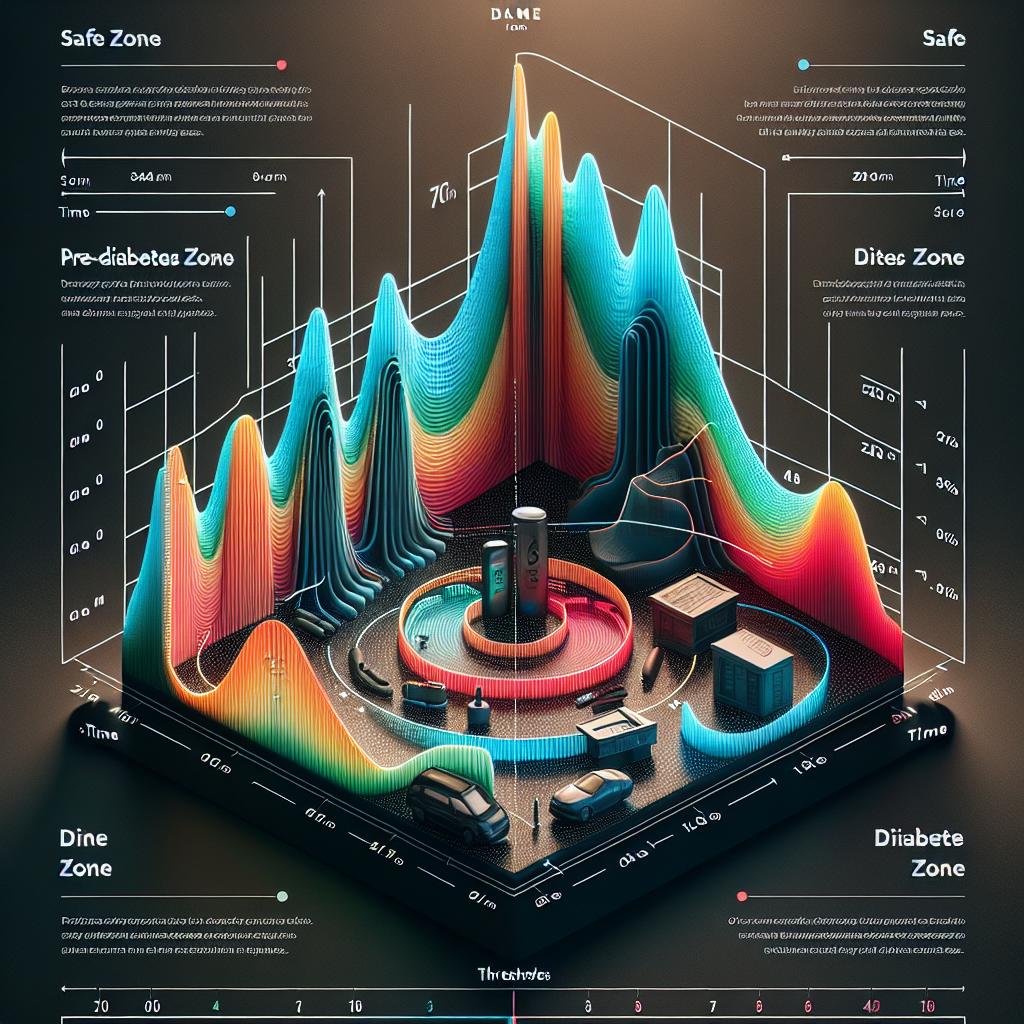
Understanding the relationship between fasting blood sugar levels and the risk of diabetes is a crucial step in early detection and management. Blood sugar readings taken after a person has not eaten for at least 8 hours—what we refer to as fasting blood sugar levels—can reveal significant insights into one’s glucose metabolism health. Recognizing the numbers that signal pre-diabetes and diabetes is the first line of defense in preventing or delaying the onset of diabetes-related complications.
For those who are concerned about their blood sugar readings, it’s important to know the thresholds that indicate a healthy range versus a signal for concern. Normal fasting blood sugar levels are typically under 100 mg/dL. When numbers start to creep up, it heralds a state of impaired fasting glucose. Individuals with fasting blood sugar levels that are between 100 to 125 mg/dL fall into the category of pre-diabetes. This is a critical stage where intervention through lifestyle changes can have a profound impact.
| Fasting Blood Sugar Level (mg/dL) | Classification |
|---|---|
| Less than 100 | Normal |
| 100 to 125 | Pre-diabetes |
| 126 and above | Diabetes |
Once the fasting blood sugar level crosses the threshold of 126 mg/dL or higher on two separate tests, diabetes is typically diagnosed. It’s essential not only to monitor blood sugar levels but also to pay attention to symptoms such as increased thirst, frequent urination, unexplained weight loss, and fatigue. These symptoms combined with blood sugar levels are robust indicators that warrant a professional medical evaluation.
Furthermore, tracking the trajectory of fasting blood sugar levels over time can offer significant insights. Spikes and patterns can be warning signs, and sometimes, even in the absence of conventional symptoms, an upward trend in fasting blood sugar can signal the need to adopt preventative measures. Diet, exercise, and in some cases, medication, can drastically alter the progression from pre-diabetes to diabetes, highlighting the power of early and proactive management.
The Importance of Consistent Monitoring of Fasting Blood Sugar
Understanding the nuances of blood glucose levels is crucial in managing and potentially preventing diabetes. Regularly tracking your morning fasting blood sugar not only gives you insight into your daily health status, but also holds the key to long-term wellness. This silent routine serves as a window to understanding how well your body is processing sugar, thereby functioning as a proactive measure in health management.
Why Regular Checks Matter
Through diligently tracking your fasting blood sugar, you are armed with personal data that assists in the early detection of pre-diabetes or diabetes. This is particularly significant because:
- It helps to assess the efficacy of diabetes management plans or medications.
- Alerts you and your healthcare provider to potential health issues before they become severe.
- Provides a baseline for how lifestyle choices affect blood sugar levels.
Decoding the Numbers
The numbers you record are more than just digits; they are indicators of your metabolic health. A normal fasting blood sugar level is typically between 70 to 99 mg/dL. Pre-diabetes is often indicated when fasting blood sugar levels consistently range from 100 to 125 mg/dL, and diabetes is suggested when levels exceed 126 mg/dL on multiple occasions. Monitoring these trends over time is indispensable for catching fluctuations and seeking timely interventions.
| Condition | Fasting Blood Sugar Level (mg/dL) |
|---|---|
| Normal | 70-99 |
| Pre-diabetes | 100-125 |
| Diabetes | ≥126 |
Staying ahead of the curve with preventive measures can significantly alter the path of your health. If detected early, pre-diabetes can often be managed or reversed through lifestyle adjustments, such as improved diet and increased physical activity. The goal is to minimize the risk of progression to diabetes and its associated complications, which can include cardiovascular disease, nerve damage, and kidney issues.
Lifestyle Interventions to Manage Fasting Blood Sugar Levels

Navigating the waters of blood sugar management requires a comprehensive approach, with lifestyle changes playing a pivotal role. When it comes to keeping fasting blood sugar levels in check, consider implementing a multi-faceted strategy that reflects a commitment to overall health and wellness.
- Diet Modification: Begin with a balanced diet rich in fiber, such as leafy greens, whole grains, and legumes. Fiber aids in slowing down glucose absorption, promoting a more gradual rise in blood sugar. Moreover, incorporating lean proteins and healthy fats can help sustain energy and curb spikes in glucose levels.
- Consistent Meal Timing: Establishing a regular eating schedule can also stabilize blood sugar. Skipping meals, especially breakfast, can lead to significant fluctuations in glucose levels. Instead, aim for smaller, more frequent meals to encourage a steady supply of energy throughout the day.
Engaging in physical activity is another cornerstone of managing blood sugar. Exercise encourages cells to use glucose for energy, effectively lowering blood sugar levels. Aim for at least 150 minutes of moderate aerobic activity per week, alongside strength training exercises twice a week to enhance insulin sensitivity. Quick bouts of exercise, like a brisk walk after meals, can be particularly effective in managing postprandial (post-meal) blood sugar levels.
Stress management is an often-overlooked facet of blood sugar control. Chronic stress triggers the release of hormones such as cortisol and adrenaline, which can increase blood sugar. Strategies like mindfulness meditation, deep breathing exercises, and yoga can be instrumental in keeping stress at bay. Encouraging a mind-body connection not only addresses glucose levels but also elevates overall well-being.
| Morning Routine | Physical Activity | Stress Reduction Technique |
| High-fiber breakfast | 30 min brisk walk | 10 min meditation |
| Hydration | Strength training | Deep breathing |
| Consistent meal timing | Post-meal stretching | Gentle yoga |
Remember, these lifestyle interventions are not a one-size-fits-all prescription but a starting point for managing fasting blood sugar levels. The journey to better health is personal and ongoing, requiring adjustments, patience, and persistence. By forging these habits, you lay the foundation for stabilizing blood sugar levels and crafting a life marked by vitality and vigor.
Medical Recommendations for Individuals with High Fasting Blood Glucose
If your fasting blood glucose levels have edged into the high territory, it’s time to take a proactive stance. Elevated levels could be indicative of prediabetes, a condition where blood sugar levels are higher than normal but not yet high enough for a diabetes diagnosis. Prediabetes is a clarion call for lifestyle changes to prevent the development of Type 2 diabetes.
Embrace Nutritional Changes
Making smarter food choices is foundational in managing your blood sugar. A diet that emphasizes the following can make a significant difference:
- Whole grains – Oats, quinoa, and whole wheat products can help regulate glucose levels.
- Fiber-rich foods – Fruits, vegetables, legumes, and nuts are not only nutritious but beneficial for blood sugar control.
- Lean proteins – Incorporate chicken, fish, and plant-based proteins to stabilize glucose.
- Avoid foods high in saturated fats, trans fats, and simple sugars, all of which can negatively impact blood glucose levels.
Regular Physical Activity
Regular exercise is another cornerstone of managing high fasting blood glucose. Aim for at least 150 minutes of moderate-intensity aerobic activity weekly, including:
- Brisk walking
- Swimming
- Cycling
Complement these activities with strength training exercises twice a week to enhance muscle mass and improve insulin sensitivity.
Monitoring and medical supervision are also crucial. Regular check-ups with your healthcare provider, coupled with self-monitoring of blood glucose levels, should be part of your routine. Your healthcare team may recommend medication if lifestyle modifications are insufficient to lower your glucose levels.
| Blood Glucose Level | Assessment |
|---|---|
| Less than 100 mg/dL | Normal |
| 100-125 mg/dL | Prediabetes |
| 126 mg/dL or higher | Diabetes |
Lastly, Stress Management plays a role since stress hormones can lead to elevated blood glucose. Techniques such as deep breathing, yoga, or meditation can be beneficial. Integrating stress-reducing practices into your daily regimen not only improves your mental well-being but can also aid in maintaining healthier blood sugar levels.
Taking immediate and consistent action can significantly influence the progression of prediabetes to Type 2 diabetes. Adhering to medical recommendations is paramount for individuals faced with the challenge of high fasting blood glucose.
Advancements in Blood Sugar Testing: Beyond the Traditional Fasting Method

When exploring the realm of diabetes detection, the evolution of blood sugar testing technology has revolutionized the way we approach this critical health metric. Traditional fasting blood glucose tests, while invaluable, only provide a snapshot of a person’s glycemic state at a single point in time. In contrast, newer methods offer a more nuanced and continuous understanding of blood sugar levels.
In contrast to the typical fasting requirement, Continuous Glucose Monitoring (CGM) systems empower individuals to track their glucose levels 24/7, without interruption. This technology utilizes a small sensor inserted under the skin that records blood sugar levels at regular intervals and sends the data to a receiver or smartphone app. Users can observe how their glucose responds to food intake, exercise, medications, and sleep in real time, offering a deeper insight into their metabolic health.
Meanwhile, advancements such as Hemoglobin A1c (HbA1c) testing have emerged as a cornerstone in diabetes management, measuring the average glucose levels over the past three months. This test does not require fasting, making it a convenient option for many. HbA1c results are reported as a percentage, with a higher percentage indicating poorer blood sugar control and a greater risk of diabetes complications.
- Flash Glucose Monitors: Wearable devices that allow users to check their glucose levels by scanning a sensor whenever needed.
- Non-Invasive Glucose Monitors: Research is ongoing into devices that can track glucose levels through methods like optical sensors, eliminating the need for finger-pricking.
In addition to individual testing methods, it is crucial to note the relational data between fasting blood glucose and other health indicators. The table below exemplifies how fasting blood sugar levels can correlate with potential health outcomes, inspiring a more comprehensive approach to diabetes detection and management.
| Fasting Blood Sugar Level (mg/dL) | Interpretation | Potential Health Outcome |
|---|---|---|
| 50-70 | Hypoglycemia | Possible insulin dysfunction or reaction to medications |
| 70-99 | Normal | Minimal risk of diabetes |
| 100-125 | Pre-diabetes | Increased risk of developing type 2 diabetes |
| 126 and above | Diabetic range | Diagnosis of diabetes or need for management review |
These insights amplify the importance of regular health assessments and personalized care plans. With the integration of non-traditional methods, we are stepping into an era where proactive monitoring could become the norm, leading to earlier interventions and more effective diabetes control.
Taking Action: Steps to Take if Your Fasting Blood Sugar Is High

When monitoring fasting blood sugar levels, it’s essential to recognize when figures stray from the normal range, indicative of potential diabetes or prediabetes. If you’ve discovered that your levels are higher than recommended, it’s time to take affirmative action. Here’s what you can do to address elevated fasting blood sugar:
Maintain a Balanced Diet
- Focus on a low glycemic index diet, choosing whole grains and fiber-rich foods, which have a more gradual impact on blood sugar levels.
- Incorporate healthy fats and lean proteins to stabilize sugar levels and provide sustained energy.
- Limit consumption of refined sugars and carbohydrates, which can cause drastic spikes in blood sugar.
Incorporate Regular Physical Activity
- Engage in at least 150 minutes of moderate aerobic activity weekly, such as brisk walking or cycling.
- Add strength-training exercises twice a week to build muscle mass, which can help regulate blood sugar levels.
- Stay consistent with your exercise routine as fluctuations in activity can affect your sugar levels.
Monitor and Track Your Blood Sugar Levels
- Keep a daily log of your fasting blood sugar readings to identify patterns and track progress.
- Consider using a continuous glucose monitoring system (CGMS) for real-time tracking and better data to manage your blood sugar.
- Regularly review your blood sugar logs with your healthcare provider to adjust your management plan as needed.
| Action | Impact on Blood Sugar | Frequency |
|---|---|---|
| Balanced Meals | Stabilizes levels | Daily |
| Physical Activity | Lowers levels | 5 days/week |
| Monitoring | Tracks patterns | Daily |
Consult with Your Healthcare Provider
- Discuss potential medications such as metformin, which can help control high fasting blood sugar levels.
- Explore lifestyle modification programs that can offer guidance and support in managing diabetes.
- Ask about referral to a dietitian or diabetes educator for personalized advice tailored to your needs.
Taking immediate steps to manage a high fasting blood sugar is crucial for long-term health. By altering your diet, increasing physical activity, diligently monitoring levels, and working closely with health professionals, you can influence your blood sugar levels positively.
Q&A
### Q&A: Diabetes Detection – The Insights of Fasting Blood Sugar
**Q1: What is fasting blood sugar and why is it important in detecting diabetes?**
Fasting blood sugar, also known as fasting blood glucose, measures the level of glucose in the blood after a period of fasting, usually overnight for at least 8 hours. This test is critical because it provides a baseline understanding of how well the body regulates glucose, which can indicate the presence of diabetes or prediabetes.
**Q2: What are the normal, prediabetes, and diabetes ranges for fasting blood sugar levels?**
Generally, fasting blood sugar levels are categorized as follows: normal (less than 100 mg/dL), prediabetes (100 to 125 mg/dL), and diabetes (126 mg/dL or higher on two separate tests). These thresholds help healthcare providers assess a patient’s glycemic control and the risk of diabetes-related complications.
**Q3: How often should one get their fasting blood sugar tested?**
Individuals over the age of 45 or those with risk factors for diabetes—such as obesity, family history, or high blood pressure—should get their fasting blood sugar levels checked at least once every three years. More frequent testing might be recommended based on the individual’s health status and initial results.
**Q4: Can fasting blood sugar levels fluctuate, and what might cause these variations?**
Yes, fasting blood sugar levels can fluctuate due to various factors, including dietary choices, physical activity, stress, illness, and the use of certain medications. It’s important to consider these variables when interpreting test results and to perform multiple tests for accurate diagnosis.
**Q5: Is fasting blood sugar the only test used to diagnose diabetes?**
No, while fasting blood sugar is a common initial test, it’s not the only diagnostic tool. Other tests include the Hemoglobin A1c test, which shows average blood sugar levels over the past three months, and the oral glucose tolerance test, measuring the body’s response to sugar over a set period.
**Q6: Are there any steps that can be taken to lower fasting blood sugar levels if they are high?**
Yes, lifestyle changes such as improving diet, increasing physical activity, losing weight, and managing stress can significantly lower fasting blood sugar levels. In some cases, healthcare providers may also prescribe medications to help control blood sugar.
**Q7: What is the role of continuous glucose monitoring in diabetes detection?**
Continuous glucose monitoring (CGM) systems provide real-time feedback on glucose levels throughout the day and night, giving a more comprehensive picture than fasting blood sugar alone. CGM can be especially useful for adjusting diabetes treatment plans and detecting patterns in blood sugar fluctuations.
**Q8: Can other health conditions affect fasting blood sugar results?**
Certain health conditions, like thyroid disorders, pancreatic issues, and hormonal imbalances, can affect fasting blood sugar results. It’s essential for healthcare providers to consider overall health when interpreting these levels and diagnosing diabetes.
**Q9: What is the significance of fasting blood sugar levels in managing existing diabetes?**
For those already diagnosed with diabetes, maintaining target fasting blood sugar levels is vital to manage the condition and prevent long-term complications. Regular monitoring helps in assessing the effectiveness of treatment plans and making necessary adjustments.
**Q10: Are there any new developments in fasting blood sugar testing technology?**
Advancements such as non-invasive blood glucose monitoring devices are in development, which may make it easier and less painful to measure fasting blood sugar levels regularly. These technologies aim to improve patient comfort and compliance with diabetes management protocols.
The Conclusion
In conclusion, fasting blood sugar tests provide a crucial window into the body’s ability to manage glucose, serving as a key tool in the early detection and management of diabetes. The implications of these results extend far beyond a single metric; they carry the weight of potential prognosis, lifestyle changes, and the necessity for medical intervention. As researchers deeper into the connections between blood glucose levels and overall health, the importance of regular screening and preemptive care cannot be understated. Individuals are encouraged to discuss their fasting blood sugar results with healthcare providers, who can offer personalized advice and strategies to mitigate the risks associated with diabetes. It’s through a combination of science, vigilance, and informed public health strategies that we can hope to curb the rising tide of this chronic disease and enhance the quality of life for those affected.